- Research
- Open access
- Published:
Video livestreaming from medical emergency callers’ smartphones to emergency medical dispatch centres: a scoping review of current uses, opportunities, and challenges
BMC Emergency Medicine volume 24, Article number: 99 (2024)
Abstract
Background
Timely dispatch of appropriate emergency medical services (EMS) resources to the scene of medical incidents, and/or provision of treatment at the scene by bystanders and medical emergency lay callers (referred to as ‘callers’ in this review) can improve patient outcomes. Currently, in dispatch systems worldwide, prioritisation of dispatch relies mostly on verbal telephone information from callers, but advances in mobile phone technology provide means for sharing video footage. This scoping review aimed to map and identify current uses, opportunities, and challenges for using video livestreaming from callers’ smartphones to emergency medical dispatch centres.
Methods
A scoping review of relevant published literature between 2007 and 2023 in the English language, searched within MEDLINE; CINAHL and PsycINFO, was descriptively synthesised, adhering to the PRISMA extension for scoping reviews.
Results
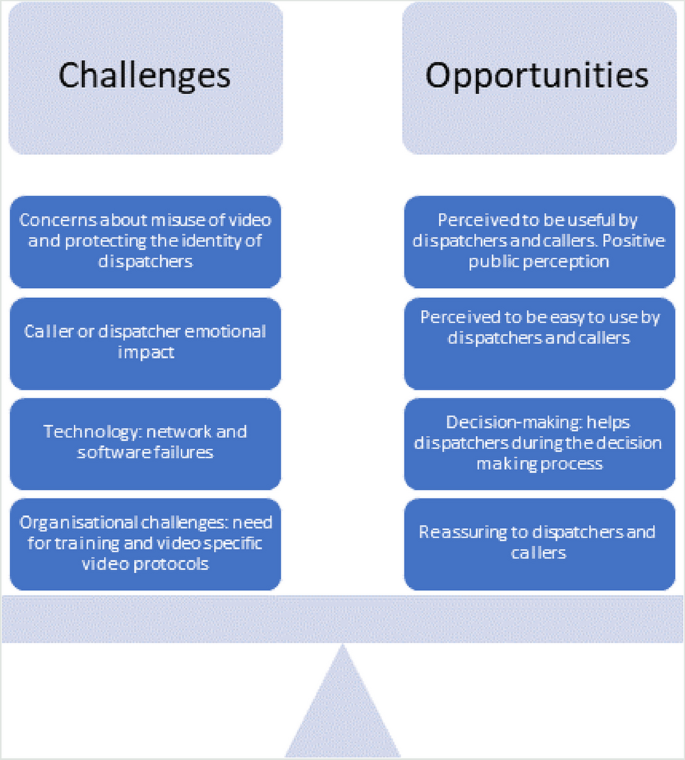
Twenty-four articles remained from the initial search of 1,565 articles. Most studies were simulation-based and focused on emergency medical dispatchers’ (referred to as ‘dispatcher/s’ in this review) assisted video cardiopulmonary resuscitation (CPR), predominantly concerned with measuring how video impacts CPR performance. Nine studies were based on real-life practice. Few studies specifically explored experiences of dispatchers or callers. Only three articles explored the impact that using video had on the dispatch of resources. Opportunities offered by video livestreaming included it being: perceived to be useful; easy to use; reassuring for both dispatchers and callers; and informing dispatcher decision-making. Challenges included the potential emotional impact for dispatchers and callers. There were also concerns about potential misuse of video, although there was no evidence that this was occurring. Evidence suggests a need for appropriate training of dispatchers and video-specific dispatch protocols.
Conclusion
Research is sparse in the context of video livestreaming. Few studies have focussed on the use of video livestreaming outside CPR provision, such as for trauma incidents, which are by their nature time-critical where visual information may offer significant benefit. Further investigation into acceptability and experience of the use of video livestreaming is warranted, to understand the potential psychological impact on dispatchers and callers.
Background
In recent years, the rapid uptake in ownership of smartphones (with integral video technology) has influenced communication in healthcare. Many healthcare providers worldwide now offer remote patient consultations via video, in particular following the COVID-19 pandemic [1].
In the emergency medical dispatch context, timely and effective dispatch of appropriate emergency medical services (EMS) resources is critical, in order to save lives [2]. However, emergency medical dispatch response has been described as the weakest link in the EMS response chain [3]. There are several different dispatch systems around the world, commonly categorised into two different systems; the criteria-based dispatch (CBD) system, and the Medical Priority Dispatch system (MPDS) [4]. Both systems rely almost exclusively on audio and verbal information from the incidents, to determine the severity of the incident and inform dispatch decision making. Evidence suggests that dispatch and resource allocation is often inappropriate (either under or over resourced) resulting in additional costs and unfavourable clinical outcomes [5]. Similarly, support and instructions to bystanders and medical emergency callers (referred to as ‘callers’ in this review) to provide help at the scene also relies predominantly on verbal (usually telephone) communication. In recent years, the uptake of smartphone ownership means that visual as well as verbal information could be used at the scene. Video livestreaming (also referred to as ‘video’ in this review) from callers’ smartphones has the potential to facilitate the timely dispatch of appropriate EMS resources and improve treatment/care delivered by bystanders and callers, and to potentially assist callers, for example when carrying out CPR [6].
Previous reviews of use of video livestreaming have focussed exclusively on its use for out-of-hospital cardiac arrest (OHCA), in particular the use of video-instructed dispatcher-assisted bystander cardiopulmonary resuscitation (CPR) (V-DACPR). These reviews have reported that dispatcher video-instructed CPR significantly improved the chest compression rate compared to the audio-instructed method [7] and that V-DACPR significantly increased the return of spontaneous circulation (ROSC) and survival to hospital discharge [8]. A further review [9] examined the scope and nature of research publications on the topic of video emergency calls but did not synthesise or thematically analyse the findings in a way that could inform practice. None of the aforementioned reviews have examined the experiences of patients, healthcare staff or callers use of video livestreaming from medical incidents. This review therefore aimed to address these deficiencies by focusing on the current uses, opportunities, and challenges for using video livestreaming from callers’ smartphones to emergency medical dispatch centres (EMDCs).
Methods
Review question
The aim of this review was to map and synthesise the published international literature regarding video livestreaming (streaming of video in real time) between callers’ smartphones and EMDCs. The review questions were:
-
1.
What are the current uses for video livestreaming from callers’ smartphones to emergency medical dispatch centres?
-
2.
What are the challenges and opportunities when using video livestreaming between emergency medical dispatch centres and callers’ smartphones?
Design
Arksey and O’Malley’s [10] five-stage scoping review method was used to guide the review. A scoping review synthesises and maps the literature in a particular area of practice, highlights the different types of evidence and identifies knowledge gaps in an emerging field. We chose to do a scoping review, as there had been limited research concerning video livestreaming in the dispatch context. There was a need to get an initial understanding of the topic area to understand the scope and nature of current evidence. We adhered to the PRISMA extension for scoping reviews [11]. The PRISMA-ScR checklist can be found in Supplementary File 1. The review protocol has not been published.
Stage 1: identifying the research question
We started by identifying the research question following initial scoping of the evidence. Due to limited number of relevant articles, it was agreed to include all types of clinical focus (such as trauma or CPR), as well as both real-life and simulation-based studies. We also agreed to focus on medical emergency lay callers only as this was our primary interest.
Study types and characteristics
This review included quantitative, qualitative, and mixed methods primary research studies, published in peer-review journals in any country in the English language between 2007 (introduction of smartphone video technology) and 2023. Reviews were excluded. Both ‘real-life’ and simulation studies were included due to the limited evidence base available for real-life studies only, and also due to the opportunity for learning from simulation settings, but papers were synthesised, and results are presented separately.
Stage 2: identifying relevant studies
MEDLINE; CINAHL and PsycINFO databases were searched in February 2023. Key words in context to the title/abstract were identified. Key terms included emergency medical dispatch, emergency medical services, air ambulance, cell phone, smartphone, telemedicine, video, livestreaming, and relevant Medical Subject Headings (MESH) using Boolean operators. An example Medline string can be found in Supplementary file 2.
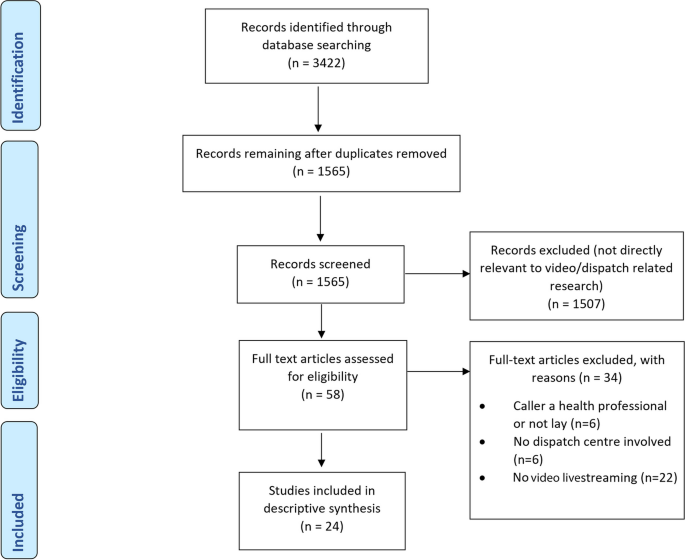
Stage 3: study selection/screening
Once the search was completed, citations were uploaded to Zotero, the reference management software and duplicates were removed resulting in 1565 papers. Title and abstracts were screened, and articles removed if they were not directly relevant to video livestreaming or dispatch. This resulted in 58 remaining articles. There was much literature covering specific video-diagnostic equipment such as laryngoscopy and other video devices used in the pre-hospital and emergency care environment, that was not relevant to this study. These were removed. Full-text review of the remaining articles (n = 58) were independently assessed (CM & LO) for eligibility using the inclusion/exclusion criteria. There was 100% agreement regarding inclusion/exclusion of these articles. In total, 24 studies were included (see Fig. 1 Prisma flowchart).
Review inclusion & exclusion criteria
Inclusion criteria included:
-
1.
Studies concerning use of video livestreaming between a lay caller and an emergency medical dispatch centre (or participant acting in the role of emergency medical dispatcher/call taker in simulation studies) AND
-
2.
Studies where the caller was a lay person (or acting in the role of a lay person in simulation studies) AND
-
3.
Studies set in an emergency medical dispatch centre or simulating that setting.
Exclusion criteria included: caller being a health professional or not a lay caller (such as the police); research not involving emergency dispatch or an emergency medical dispatch centre; or did not involve video livestreaming.
Stage 4: charting the data/data extraction
Data were extracted independently by the first author (CM all articles) and repeated by one of two research paramedic co-authors (AC and OF, each randomly allocated 50% of articles) using a bespoke data extraction tables in Word (see Tables 1 and 2). These were designed to comprehensively capture generic study information (i.e., aims, objectives, study settings/country etc.), as well as key study characteristics such as design/methodology, and information about the study population. We also extracted information about whether the study was real-life or simulation, whether the video communication was one- or two-way, study clinical focus, and reported key challenges and opportunities to using video livestreaming. Data extraction was compared between the three reviewers and any differences were discussed and agreed between reviewers. We did not appraise the methodological quality of the articles, consistent with scoping review guidance [10].
Stage 5: collating, summarising and reporting the results
The findings were synthesised descriptively (real-life and simulation separately) according to Arksey and O’Malley’s [10] framework using thematic analysis to answer the review questions. Key themes were identified (and sub-themes). Results were organised and mapped according to the review questions (opportunities and challenges) for each theme. This process was iterative and involved updating data extraction tables and additional re-reading of the papers to make sure that all relevant data relating to the themes or main themes had been included in the analysis.
Results
In total, 24 studies were included (see Fig. 1, PRISMA Diagram). Nine of the studies were based on real-life clinical practice (see Table 1) and fifteen were simulation studies (see Table 2). Ten of the fifteen simulation studies used comparison groups (nine used audio/voice calls and one study suboptimal light and sound conditions) as part of the research design. Only two of the real-life studies [14, 15] used comparison groups, both focussing on dispatcher-assisted CPR clinical outcomes. In total, half of the included 24 studies used comparison groups and the other half relied on less robust study designs and used self-report data only. Most studies were conducted in Norway (n = 6) and South Korea (n = 6), followed by Belgium (n = 2), Denmark (n = 2), England (n = 2), Germany (n = 2). One study was conducted in each of the following countries: Canada [17], Israel [30], Japan [25] and Taiwan [33]. Nine of the studies reported using one-way video (caller not able to see the dispatcher), seven studies used two-way video communication (caller and dispatcher could see each other) and the remainder did not report mode of use (see Tables 1 and 2). Most included studies were quantitative (n = 17), four were qualitative, and three were mixed methods. The design, source characteristics and results are summarised in Table 1 (real-life studies) and Table 2 (simulation studies). The results of the thematic synthesis of findings are organised under four main heading, and key findings are presented in Fig. 2 (below).
Current uses of video livestreaming between callers and emergency medical dispatch centres
In the nine real-life studies, three focussed on CPR only [14,15,16] and six had a broad clinical focus (with limited further detail included in the papers) ranging from trauma incidents to lower priority calls (see Table 1). These studies were undertaken in various countries including Norway, where a study had piloted video in four medical emergency medical communication centres [13]; Denmark [6], where dispatchers were able to decide when to use video streaming, and reported that video was used more frequently in cases with sick children or unconscious patients; and Seoul, South Korea, video was added to their dispatcher-assisted CPR programme in 2017 [15].
In the 14 simulation studies, ten focused on dispatcher-assisted CPR (see Table 2), two on incidents simulating foreign bodies in mouth (used as simulation scenario) [25, 29], and two investigated the feasibility of using video call to guide lay people using automated external defibrillators (AEDs) following simulated cardiac arrests [20, 34]. The majority of simulation studies focussed on adult casualties, but two used paediatric cases [25, 31].
Emergency medical dispatchers’ perspectives: opportunities and challenges
Over half of the papers (n = 14/24) included some information (though few had this as the study focus) on the views of the dispatchers (or those acting as dispatchers in simulation studies) about video livestreaming. Perspectives reported in these papers were overwhelmingly positive, with dispatchers reporting video livestreaming to be acceptable and easy to use, reporting various benefits of video livestreaming including its use as an aid for emergency medical dispatch decision-making, video dispatcher-assisted CPR improving caller technique when performing CPR, more accurate patient assessment and/or supporting better/more effective decision-making. Challenges included the potential emotional impact of seeing traumatic incidents that dispatchers would normally only ‘hear’, the potential for additional fatigue and workload, and concerns about the potential misuse of video were also reported. There was no evidence provided in any of the papers to support these concerns other than perceived potential impact. However in one real-life Norwegian study [18] dispatchers referred to colleagues having visual impressions that they were not prepared for.
Real-life studies
Clinicians reported that video ‘consultations’ (following medical emergency calls) were superior to audio only [12], easy to use [26], and that they wanted to use video in the future, especially for dispatcher-assisted CPR [23]. Dispatchers reported finding video livestreaming extremely useful [6], that it improved communication with callers [13], and also provided dispatchers with general reassurance in their decision-making [13]. Additional benefits included the ability to make a more thorough assessment of patients’ needs compared to telephone alone [12, 13]. Dispatchers also reported that video streaming helped them assess the quality of CPR, obstructed airways, or position of the patient [16], and more easily evaluate different situational elements (such as bleeding or context of incidents) [18]. There was some preliminary evidence that video livestreaming impacted positively on dispatch decisions, prioritisation, and/or resource allocation. For example, in one study the medical dispatchers changed the dispatch response in approximately one quarter of calls after viewing the video [18]. In another study, dispatchers reported that video supported more precise resource allocation [13]. Challenges reported in real-life studies (self-report) included the potential emotional impact of viewing video footage [18], in particular when the call involved children [13]. In this Norwegian study, dispatchers could choose to use live video as an additional tool for communication, and a few of the dispatchers interviewed described that they felt uncomfortable activating video when children were involved [13]. Additionally, some dispatchers reported in interviews that using video livestreaming was more time-consuming and might divert their attention, potentially leading them to forget other tasks [13], increased their workload [6] and created potential information overload, although the dispatchers in the study [17] had never used video streaming.
Simulation studies
In simulation studies, video was reported to be superior to audio alone, helped to clarify misunderstandings with callers and motivated callers to continue with CPR [22,23,24]. Dispatchers reported that video helped them to save time gathering information from the callers, as they did not need to ask all of the standard questions [26]. Half of the dispatchers in a German simulation study (51%) agreed that video “supported them in making a diagnosis” [24]. Only two of the simulation studies covered challenges with video streaming from the dispatchers’ perspective [23, 26]. Ecker et al. [23] surveyed dispatchers following simulated cardiac arrests and 30% agreed that they found using live video more stressful or exhausting compared to normal telephone (audio) protocol (simulation used video only, we make the assumption that the dispatchers compared this to their normal audio practice). Similarly, in Johnsen and Bolle’s [26] study, some of the dispatchers interviewed felt that video had the potential to cause extra strain and stress, for example, when witnessing deaths. The dispatchers in this simulation study were also worried about the videos potentially being misused and distributed by callers to mass media, as well as the loss of identity protection, as in this study dispatchers were visible to callers [26].
Caller perspectives: opportunities and challenges
Ten studies included perspectives from or regarding the callers (or those acting as callers in simulation studies). Most of these studies (n = 6) reported proxy views of the callers’ perspectives from dispatchers, for example describing their experience of dealing with the caller, and sometimes speculating what callers may do if they added video to a call. The evidence in these papers suggested that callers in both real-life and simulation studies had positive attitudes and experiences of video livestreaming. On the basis of these studies, video streaming technology appears largely acceptable to callers, and few challenges were reported. Callers were generally positive, reported feeling reassured by the video, comforted by not being alone, and satisfied with the help they received. Very few challenges from the caller perspective were reported in the included articles, but some contained instances when video was reported to potentially increase callers’ stress, was disruptive or divided/diverted attention from the scene.
Real-life studies
Four of the real-life studies included assessment of acceptability to callers or satisfaction with the use of video livestreaming (all these studies used self-report, see further below). Callers found video reassuring, comforting and not feeling “alone” [13], and enabled them to express their needs in a better way [12]. Linderoth et al. [6], surveyed callers in Denmark following real-life emergencies using live video, and nearly all (97.3%) reported that live video should be implemented. Although Ter Avest et al. [19] did not specifically ask callers about their experience, all of the callers in the study (n = 21) were willing to attempt video livestreaming and the dispatchers reported that all callers were able to follow their instructions. Dispatchers rated their perception of callers’ acceptability of using video as “excellent” in all calls [19]. An interesting observation was made in a real-life study [14] in Seoul, South Korea, where video-instructed dispatcher-assisted CPR has been well established in practice for some time. It was noted anecdotally that increasing public awareness of its use through national news items reduced the tendency of callers to reject the change from audio to video instructions, hence improving acceptability. Challenges reported in real-life studies included dispatchers perceiving that, at times, the use of video increased callers’ stress [13] and some callers reporting technical difficulties such as video freezing [12].
Simulation studies
As per the real-life studies above, callers in simulation studies have reported that sharing the scene with the dispatchers through video gave them comfort that they were not alone [27] and feeling reassured that dispatchers “could see whether I did the right thing” [12]. Most of the callers in Bolle’s et al.’s [21] Norwegian study reported that using video was better than standard telephones during medical simulated emergencies and improved their confidence when performing CPR. Challenges reported in simulation studies were very rare, although one survey participant (caller) in a Norwegian simulation study reported that they were concentrating more on recording the video than the situation [21]. In a Korean study [27], callers reported being concerned about how they would manage the situation if connection was lost during a video call, though none of them reported that this had happened.
Organisational perspectives: opportunities and challenges
Although none of the studies specifically focused on organisational issues, or systematically collected such data, ten studies offered important insights into the challenges and opportunities of using video livestreaming from an organisational perspective. The reported evidence in these papers suggest a need for training, video-specific protocols and a need to consider how best to implement video livestreaming into existing organisational structures. No specific organisational benefits were reported in the studies, although the benefits reported by callers and dispatchers earlier is suggestive of benefits to the organisation, for example by improving resource allocation.
Real-life studies
Linderoth et al. [6] reported that video livestreaming could potentially interfere with existing symptom-based dispatch protocols; it was observed by the researchers that some of the dispatchers appeared to avoid using video livestreaming during particularly busy times. Other studies have supported the need to implement dispatch protocols and guidelines for the specific purpose of video livestreaming, as well as highlighting the need to fully integrate video features into existing IT-systems and processes [18]. Dispatchers have highlighted the need for experience in using the new technology [13] and the authors in another study suggested that the helicopter emergency medical service (HEMS) dispatchers in their pilot study needed to be provided with adequate support when potentially witnessing images that were unusual in their role [19]. Although not specifically measured, the authors in one of the real-life studies noted that there had been positive effects between the dispatcher and caller via video-instructed CPR, such as providing real-time feedback [14].
Simulation studies
Similar findings about the importance of protocols and training were reported in the simulation studies. Ecker et al. [24] argued that training and additional support is needed to help dispatchers to develop new skills in using video. In another study, it was argued that training was also needed to help dispatchers integrate video CPR into existing workflows [23]. Stipulante et al. [32] developed and validated a protocol for video-assisted CPR and the new protocol supported improvement in some of the CPR performance indicators. Similarly, Perry et al. [30] used a ‘filming protocol’ for dispatcher video-assisted CPR and findings showed that the bespoke protocol improved CPR effectiveness. Perry et al. [30] also stressed that to maximise the use of the new technology, special attention is needed to implement video streaming in practice.
Technological factors: opportunities and challenges
Ten studies (five real-life and five simulation studies) included findings regarding the streaming technology, such as impact of lighting conditions, visibility, and sound quality. The few technical challenges that were identified in this review included problems with SMS/links, the positioning of the video camera, and lack of network coverage, although this was rare. Despite some difficulties in relation to these issues, in the majority of uses within all studies (both real-life and simulation studies), few technical barriers were reported. Both real-life and simulation studies reported high video call success connection rates.
Real-life studies
Two studies reported video call success rates; nineteen out of 21 calls were successful in obtaining video from the scene in a small feasibility study [19] and live video succeeded in over 80% of calls (N = 838) in a study in Denmark [6]. The small number of unsuccessful calls in these two studies were reported to be due to technical issues, lack of caller skills or callers not receiving the SMS with the link to activate the video. Some dispatchers in a Canadian study were worried about potential technical challenges with the CAD (computer aided dispatch) system and transferring calls, although they had never personally used video for dispatch purposes [17].
Simulation studies
One study [29] specifically investigated using video livestreaming under different sound and light conditions. The authors concluded that video calls can be used successfully in suboptimal conditions, such as during night-time, poor lighting, and noisy conditions. Dispatchers in a simulation study carried out in Germany judged both the video audio quality and the video quality as excellent in nearly all calls. Several of the simulation studies explored video call success connection rates. Video calls succeeded in 76% of calls in a Japanese study [25] and in 85% of calls in a German study [24]. The technical reasons for unsuccessful calls were due to network failure, application software failures, and IT server problems. Dispatchers interviewed in a Norwegian study [26] reported some technical challenges, such as the image quality depending on how steadily the camera was held. Others reflected that if the call had been outside, the wind and noise from people and cars may be disruptive [26].
Discussion
Our review has shown that despite the increased uptake of video livestreaming in emergency services, the evidence base remains sparse. Much of the previous research focuses on one aspect of emergency care, the use of CPR, and many of the studies are simulation-based rather than real-life clinical settings. Furthermore, methodological limitations have made attribution of findings to the use of video challenging, such as the lack of control groups or use of randomised designs, and there is a reliance on self-reported data.
Nevertheless, with these caveats, evidence from this synthesis suggests that video streaming is acceptable and easy to use to both callers and dispatchers and could be beneficial in relation to supporting video dispatcher-assisted CPR, and reassuring dispatchers and callers. There is limited research regarding callers overall experiences of calling EMDCs, but a literature review [35] found that bystanders at motor vehicle accidents often experienced fear of liability or fear of further harming the victim/patient. Video livestreaming offering reassurance to callers may provide additional benefits in these situations. Our results highlighted that callers were generally positive to video livestreaming, but most of the evidence relied on proxy views of the callers’ perspectives from dispatchers. Only two of the real-life studies surveyed callers [6, 12] regarding their experience, and response rates were relatively low (below 22% in both studies), making it challenging to conclude what impact that video livestreaming may have on callers. Evidence from our review also suggests that video livestreaming could improve dispatchers’ clinical assessment and decision-making. Currently, dispatchers’ situational awareness and decision-making skills rely on the ability to obtain information about the incident and on their verbal communication skills [36]. Our review did not find any evidence of how or why video livestreaming impacts on decision-making processes, highlighting a gap in evidence.
Challenges included potential for additional dispatcher workload, stress, and the emotional impact of viewing video footage. In the simulation studies it was not possible to decipher whether the stress was partly induced by the simulated scenarios. Research has shown that simulation often creates anxiety and stress in participants [37]. Nevertheless, dispatchers are known to be at increased risk of stress, anxiety and depression [38]. New working practises, such a video livestreaming, need to consider approaches to minimise potential additional stress to dispatchers.
Our review raised important questions whether video livestreaming should be used selectively for specific conditions, high/low acuity, or for every call. As outlined in our results, most of the included studies investigated the use of video livestreaming for CPR only, reporting a range of positive outcomes [14,15,16, 23, 26], indicating usefulness in this area. In one of the real-life studies [6] the dispatchers chose when to initiate video livestreaming. Video was used more frequently with children and unconscious patients, described as “unable to talk for themselves”. Another study [12] investigated the use of video triage for low-acuity calls (such as diarrhoea, vomiting, and urine infection) during covid-19. Over half of the category 5 (low acuity) calls were upgraded after the video consultation, representing a potential important use for low-acuity calls. Further research is needed to understand for what type of calls video livestreaming is most beneficial.
The results of our review highlighted several additional significant topics that need to be considered when conducting research and implementing video livestreaming into practice. First, improving public awareness about the use of livestreaming by emergency services may help to increase caller acceptance and compliance rates, as highlighted in a study in South Korea, where dispatcher-assisted video CPR has been in use for some time [14]. Second, a number of the studies [13, 19] also emphasised the importance of training dispatchers in using video technology. Our results indicate that dispatchers may need training in developing new skills in using video livestreaming and to help them integrate video into existing workflows. Internationally, there are several types of emergency medical dispatch systems and the professional background of call takers and dispatchers varies from no healthcare training to being trained health professionals with extensive experience [4]. The impact of professional/clinical backgrounds on using livestreaming is currently unknown. Future implementation of video livestreaming in this context is likely to require bespoke training programmes that consider local and national medical emergency systems and processes. Indeed, Linderoth et al. [6] argued that dispatcher training to use video livestreaming needs a comprehensive approach as the additional visual information may add further complexity to the decision-making process. Third, our review also drew attention to the need to carefully review dispatch protocols and organisational systems to ensure that they are compatible with video livestreaming technology. Fourth, dispatchers in one Norwegian study [26] voiced concern about the potential misuse of the videos and the loss of identity protection. Two-way video communication (where caller and dispatcher could see each other) was used in seven of the studies, raising potential concerns regarding privacy and identity for dispatchers. Overall, our review found limited information regarding the ethical aspects of video livestreaming from medical emergency callers’ smartphones. Many of the studies had local research ethical review only, or ethical review approval ‘waived’ and provided limited information regarding the caller and/or patient consent processes. Two of the studies [13, 18] mentioned that dispatchers told callers during the consent process that the video was not being stored and callers’ smartphones could not be accessed. Future research needs to explore key ethical issues, such as privacy, dignity, information-governance and provide recommendations regarding how to best approach caller and patient consent.
Key gaps identified by our review were that few studies included data collected specifically from the callers and none of the studies included any health economic analysis. Only three of the studies included analysis of change in dispatch decisions regarding resources sent to scenes of incidents. There was also a lack of qualitative studies exploring the experiences of callers, dispatchers, and patients. Future research would benefit from including ethnographic observations ‘in the field’, taking account of important organisational factors and prevailing cultures, as these are known to have an impact on the implementation of new technologies [39], such as video livestreaming.
Strengths and limitations
The review used a comprehensive search strategy that enabled capture and synthesis of international evidence related to the use of video livestreaming in this context. It uniquely synthesises the potential benefits, challenges and opportunities to inform future research and practice. The review included both real-life and simulation studies and presented the results separately which allowed a systematic overview of evidence base. The review was limited to papers written in the English Language and it is possible that it therefore omits some key international literature. The chosen search terms may have limited inclusion, although a broader search strategy was initially used, in order to determine how best to use limiters to only focus on relevant literature.
Conclusion
The evidence base into the use of video livestreaming in this context is sparse. There are few studies of real-life practice, studies generally employ weak study designs, and caller perspectives are lacking. Over half of the studies focussed on dispatcher-assisted CPR. Nevertheless, there is growing evidence of potential opportunities to using this technology, including for improved clinical assessment and decision-making. These need to be balanced with consideration of the challenges uncovered in this review. Further well-designed robust research is needed, in particular into the experiences, acceptability and attitudes of both callers and dispatchers in real-life studies, and robust evidence of the effectiveness and cost effectiveness of implementing such technologies.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Abbreviations
- AED:
-
Automated External Defibrillators
- CAD:
-
Computer Aided Dispatch
- CBD:
-
Criteria-based dispatch
- CPR:
-
Cardiopulmonary resuscitation
- EMDC:
-
Emergency Medical Dispatch Centre
- EMS:
-
Emergency Medical Services
- MESH:
-
Medical Subject Headings
- MPDS:
-
Medical Priority Dispatch System
- OHCA:
-
Out-of-hospital cardiac arrest
- ROSC:
-
Return of Spontaneous Circulation
- V-CPR:
-
Video CPR
- V-DACPR:
-
Video-instructed dispatcher-assisted bystander cardiopulmonary resuscitation
References
Greenhalgh T, Wherton J, Shaw S, Morrison C. Video consultations for covid-19. BMJ. 2020;368:m998.
Duke M, Tatum D, Sexton K, Stuke L, Robertson R, Sutherland M, et al. When minutes fly by: what is the true “golden hour” for air care? Am Surg. 2018;84:862–7.
Schellhaaß A, Popp E. [Air rescue: current significance and practical issues]. Anaesthesist. 2014;63:971–80; quiz 981–2.
Bohm K, Kurland L. The accuracy of medical dispatch - a systematic review. Scand J Trauma Resusc Emerg Med. 2018;26:94.
Eaton G, Brown S, Raitt J. HEMS dispatch: a systematic review. Trauma. 2018;20:3–10.
Linderoth G, Lippert F, Østergaard D, Ersbøll AK, Meyhoff CS, Folke F, et al. Live video from bystanders’ smartphones to medical dispatchers in real emergencies. BMC Emerg Med. 2021;21:101.
Lin YY, Chiang WC, Hsieh MJ, Sun JT, Chang YC, Ma MHM. Quality of audio-assisted versus video-assisted dispatcher-instructed bystander cardiopulmonary resuscitation: a systematic review and meta-analysis. Resuscitation. 2018;123:77–85.
Bielski K, Böttiger BW, Pruc M, Gasecka A, Sieminski M, Jaguszewski MJ, et al. Outcomes of audio-instructed and video-instructed dispatcher-assisted cardiopulmonary resuscitation: a systematic review and meta-analysis. Ann Med. 2022;54:464–71.
Sýkora R, Peřan D, Renza M, Bradna J, Smetana J, Duška F. Video emergency calls in medical dispatching: a scoping review. Prehosp Disaster Med. 2022;37:819–26.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8:19–32.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169:467–73.
Bell F, Pilbery R, Connell R, Fletcher D, Leatherland T, Cottrell L, et al. The acceptability and safety of video triage for ambulance service patients and clinicians during the COVID-19 pandemic. Br Paramedic J. 2021;6:49–58.
Idland S, Iversen E, Brattebø G, Kramer-Johansen J, Hjortdahl M. From hearing to seeing: medical dispatchers’ experience with use of video streaming in medical emergency calls – a qualitative study. BMJ Open. 2022;12:e063395.
Lee HS, You K, Jeon JP, Kim C, Kim S. The effect of video-instructed versus audio-instructed dispatcher-assisted cardiopulmonary resuscitation on patient outcomes following out of hospital cardiac arrest in Seoul. Sci Rep. 2021;11:15555.
Lee SY, Song KJ, Shin SD, Hong KJ, Kim TH. Comparison of the effects of audio-instructed and video-instructed dispatcher-assisted cardiopulmonary resuscitation on resuscitation outcomes after out-of-hospital cardiac arrest. Resuscitation. 2020;147:12–20.
Linderoth G, Rosenkrantz O, Lippert F, Østergaard D, Ersbøll AK, Meyhoff CS, et al. Live video from bystanders’ smartphones to improve cardiopulmonary resuscitation. Resuscitation. 2021;168:35–43.
Neustaedter C, Jones B, O’Hara K, Sellen A. The benefits and challenges of video calling for emergency situations. In: Proceedings of the 2018 CHI Conference on Human Factors in Computing Systems. New York: Association for Computing Machinery; 2018. p. 1–13.
Steen-Tveit K, Munkvold BE, Radianti J. Using live video for communication between lay bystanders and emergency dispatchers in command and control centres. Int J Emerg Manag. 2021;17:154–76.
Ter Avest E, Lambert E, de Coverly R, Tucker H, Griggs J, Wilson MH, et al. Live video footage from scene to aid helicopter emergency medical service dispatch: a feasibility study. Scand J Trauma Resusc Emerg Med. 2019;27:55.
Bang JY, Cho Y, Cho GC, Lee J, Kim IY. Can mobile videocall assist laypersons’ use of automated external defibrillators? A randomized simulation study and qualitative analysis. Biomed Res Int. 2020;2020:1–7.
Bolle SR, Johnsen E, Gilbert M. Video calls for dispatcher-assisted cardiopulmonary resuscitation can improve the confidence of lay rescuers–surveys after simulated cardiac arrest. J Telemed Telecare. 2011;17:88–92.
Bolle SR, Scholl J, Gilbert M. Can video mobile phones improve CPR quality when used for dispatcher assistance during simulated cardiac arrest? Acta Anaesthesiol Scand. 2009;53:116–20.
Ecker H, Wingen S, Hagemeier A, Plata C, Bottiger B, Wetsch W. Dispatcher self-assessment and attitude toward video assistance as a new tool in simulated cardiopulmonary resuscitation. WestJEM. 2022;23:229–34.
Ecker H, Wingen S, Hamacher S, Lindacher F, Böttiger BW, Wetsch WA. Evaluation of CPR quality via smartphone with a video livestream - a study in a metropolitan area. Prehosp Emerg Care. 2021;25:76–81.
Igarashi Y, Suzuki K, Norii T, Motomura T, Yoshino Y, Kitagoya Y, et al. Do video calls improve dispatcher-assisted first aid for infants with foreign body airway obstruction? A randomized controlled trial/simulation study. J Nippon Med Sch. 2022;89:526–32.
Johnsen E, Bolle SR. To see or not to see—better dispatcher-assisted CPR with video-calls? A qualitative study based on simulated trials. Resuscitation. 2008;78:320–6.
Kim HJ, Kim JH, Park D. Comparing audio- and video-delivered instructions in dispatcher-assisted cardiopulmonary resuscitation with drone-delivered automatic external defibrillator: a mixed methods simulation study. PeerJ. 2021;9: e11761.
Lee SGW, Kim TH, Lee HS, Shin SD, Song KJ, Hong KJ, et al. Efficacy of a new dispatcher-assisted cardiopulmonary resuscitation protocol with audio call-to-video call transition. Am J Emerg Med. 2021;44:26–32.
Melbye S, Hotvedt M, Bolle SR. Mobile videoconferencing for enhanced emergency medical communication - a shot in the dark or a walk in the park? –– A simulation study. Scand J Trauma Resusc Emerg Med. 2014;22:35.
Perry O, Wacht O, Jaffe E, Sinuany-Stern Z, Bitan Y. Using a filming protocol to improve video-instructed cardiopulmonary resuscitation. Technol Health Care. 2020;28:213–20.
Peters M, Stipulante S, Cloes V, Mulder A, Lebrun F, Donneau AF, et al. Can video assistance improve the quality of pediatric dispatcher-assisted cardiopulmonary resuscitation? Pediatr Emerg Care. 2022;38:e451-457.
Stipulante S, Delfosse AS, Donneau AF, Hartsein G, Haus S, D’Orio V, et al. Interactive videoconferencing versus audio telephone calls for dispatcher-assisted cardiopulmonary resuscitation using the ALERT algorithm: a randomized trial. Eur J Emerg Med. 2016;23:418–24.
Yang C-W, Wang H-C, Chiang W-C, Chang W-T, Yen Z-S, Chen S-Y, et al. Impact of adding video communication to dispatch instructions on the quality of rescue breathing in simulated cardiac arrests–a randomized controlled study. Resuscitation. 2008;78:327–32.
You JS, Park S, Chung SP, Park JW. Performance of cellular phones with video telephony in the use of automated external defibrillators by untrained laypersons. Emerg Med J. 2008;25:597–600.
Hall A, Wooton K, Hutton A. Bystander Experiences at and after a Motor Vehicle Accident: A review of the literature. Australas J Paramed. 2013;10:1–10.
Møller TP, Jensen HG, Viereck S, Lippert F, Østergaaard D. Medical dispatchers’ perception of the interaction with the caller during emergency calls - a qualitative study. Scand J Trauma Resusc Emerg Med. 2021;29:45.
Paskins Z, Peile E. Final year medical students’ views on simulation-based teaching: a comparison with the best evidence medical education systematic review. Med Teach. 2010;32:569–77.
Smith EC, Holmes L, Burkle FM. Exploring the physical and mental health challenges associated with emergency service call-taking and dispatching: a review of the literature. Prehosp Disaster Med. 2019;34:619–24.
Jennett P, Yeo M, Pauls M, Graham J. Organizational readiness for telemedicine: implications for success and failure. J Telemed Telecare. 2003;9(2 suppl):27–30.
Acknowledgements
Extended thank you to Freda Mold for assistance with search strategy and search strings. This review was completed as part of the SEE-IT trial (https://fundingawards.nihr.ac.uk/award/NIHR130811). The SEE-IT trial group also include: Kate Bennett-Eastley, Mark Cropley, Heather Gage, Matthew Glover, Janet Holah, Richard Lyon, Craig Mortimer, Simon S Skene and Julia Williams.
Funding
This project was funded by the National Institute for Health and Care Research (NIHR130811) Health and Social Care Delivery Research programme and will be published in Health and Social Care Delivery Research. See the NIHR Journals Library website for further project information.
Author information
Authors and Affiliations
Contributions
CM, JM, LO and CT made substantial contributions to the conception of the review and the development of the review focus. CM carried out all database searches. CM and LO independently assessed articles for eligibility using the inclusion and exclusion criteria. CM, AC, OF and SM extracted the data from the final included full text articles. The first draft of the manuscript was drafted by CM and CT, and critically reviewed by all other authors named. All authors agree with manuscript results and conclusion. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval not required for this review and the information included is publicly available.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Magnusson, C., Ollis, L., Munro, S. et al. Video livestreaming from medical emergency callers’ smartphones to emergency medical dispatch centres: a scoping review of current uses, opportunities, and challenges. BMC Emerg Med 24, 99 (2024). https://doi.org/10.1186/s12873-024-01015-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12873-024-01015-9